Republican Senator Chuck Grassley Sets Sights on Medicare Advantage
Sen. Chuck Grassley, a longtime Medicare Advantage advocate, demands answers from UnitedHealth Group over allegations of overbilling.
For years, whistleblowers, independent researchers, and journalists have warned about how Medicare Advantage (MA) plans manipulate risk scores to overcharge taxpayers. Now, a powerful Republican senator — one of the original champions of the program — is demanding answers.

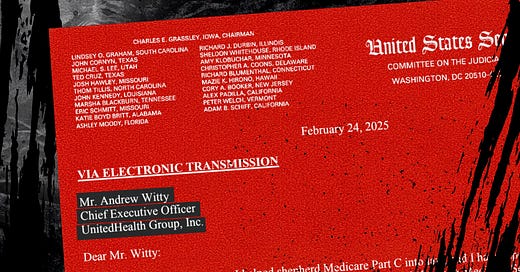
On Monday, Senator Chuck Grassley (R-Iowa) sent a letter to UnitedHealth Group CEO Sir. Andrew Witty, calling out the company for its alleged role in widespread Medicare Advantage overbilling. Citing a recent Wall Street Journal investigation, Grassley’s letter underscores what many of us have been shouting from the rooftops: Medicare Advantage is riddled with waste and abuse — and it’s costing taxpayers billions.
The $8.7 Billion Question
Grassley’s letter references findings from a Wall Street Journal story, which reported that the Department of Justice (DOJ) is investigating UnitedHealth’s Medicare billing practices. At the center of the probe is UnitedHealth’s use of in-home health risk assessments (HRAs) and chart reviews to justify additional diagnoses — often obscure, questionable, or outright inaccurate, according to the Journal’s investigation into the company’s business practices—that increase Medicare payments to the company.
According to the Journal, these tactics led to a staggering $8.7 billion in extra payments to UnitedHealth in 2021 alone. The Health and Human Services Office of Inspector General (HHS OIG) has also flagged UnitedHealth as the top beneficiary of these billing practices, raising questions about the legitimacy of these diagnoses and whether patients actually receive necessary follow-up care.
A Republican Who Helped Create Medicare Advantage
Grassley’s inquiry is significant for a few reasons.
First, he’s no Medicare Advantage skeptic — he was instrumental in creating Medicare Part C, which later became the modern Medicare Advantage program. For years, he defended the private insurance industry’s role in administering Medicare benefits, but now he is demanding information from the biggest Medicare Advantage insurer, and that represents an important shift in a Congress now fully controlled by Republicans.
Grassley’s letter demands that UnitedHealth turn over key documents, including internal audits, compliance reports, training manuals, and software data related to its diagnosis practices. He has set a March 10 deadline for the company to respond. Here are the questions and requests Grassley listed in his letter to Witty:
1. What steps has UnitedHealth Group taken to review all diagnoses submitted to CMS for its Medicare Advantage enrollees (“enrollees”) that were identified only by HRAs or chart reviews (either manual or artificial intelligence) and to identify all submitted diagnoses that are obscure, irrelevant, or inaccurate? Quantify the number and amount of inappropriate payments identified as a result of these actions. Provide all records.
2. Provide all records that relate to the compliance program that UnitedHealth Group had in place from 2019-2024 to monitor the accuracy and appropriateness of the diagnosis codes submitted to CMS for enrollees, including the design and results of all audits conducted.
3. Provide all training manuals and guidance documents for conducting HRAs and manual chart reviews, a list of all software used during the course of an HRA and a manual chart review, and the logic rules for all electronic decision support tools embedded in the software. Does UnitedHealth Group use artificial intelligence to conduct the aforementioned processes? Are all diagnoses identified by artificial intelligence confirmed by a trained medical record reviewer?
4. Provide all policies and procedures for obtaining diagnostic confirmation from an enrollee’s primary care provider and ensuring the receipt of treatment for a new diagnosis identified by an HRA or a chart review. Provide all documentation related to compliance audits of this process.
Second, his letter comes as the Republican-led Congress is seeking spending cuts. While many Republicans have traditionally been staunch defenders of Medicare Advantage, Grassley’s willingness to scrutinize insurers’ billing practices suggests a potential turning point. As Rep. Greg Murphy (R-N.C.), a physician, bluntly put it: “We’re seeing such abuse to the system that nobody really can turn a blind eye to this.”
The Industry’s Response
UnitedHealth denies any wrongdoing. In a statement, the company claimed it welcomes the opportunity to share “the facts” with Grassley and accused the Wall Street Journal of leading a “misinformation campaign.” While the company insists that Medicare Advantage delivers better health outcomes and lower costs, those claims are getting harder to defend in the face of mounting evidence to the contrary.
A Reckoning for Medicare Advantage?
The timing of Grassley’s inquiry is crucial. As the Congressional Budget Office (CBO) recently projected, just eliminating payments for diagnoses detected only through home visits could save taxpayers $124 billion over the next decade. With Republicans searching for ways to reduce government spending, Medicare Advantage’s rampant overpayments may finally be getting the scrutiny they deserve.
As someone who once worked inside the health insurance industry, I’ve seen how insurers game the system to boost profits. Grassley’s willingness to take the industry leader to task is a major development and a sign that Medicare Advantage’s free ride might be coming to an end.




The only way anyone could ever have supported Medicare Advantage is to be willfully ignorant of the structural defects of Medicare Advantage. Primary care providers are the gate keepers, insurers limit networks, then overcharge Medicare.
This is a perfect example of what happens when you privatize any service, they exploit the reimbursement system and people enrolled. Here comes corruption and they new Trump/Musk administration moving in that direction with many government systems.