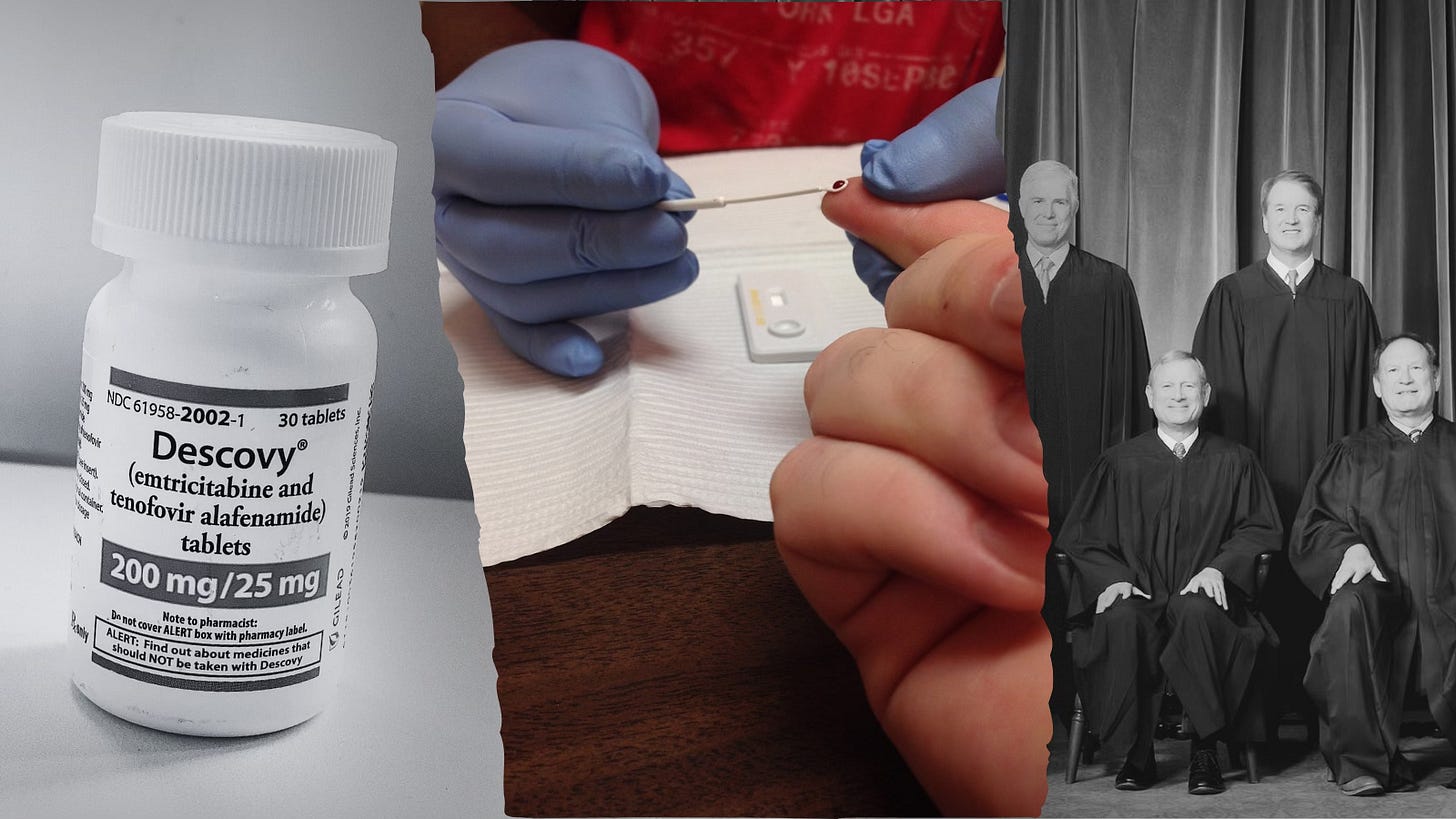
Big Health Insurers Make It Harder (and Pricier) to Stay HIV-Free – and SCOTUS Could Make Things Worse
Insurers could help you stay HIV-free, but where’s the money in that?
In a world where recent medical breakthroughs have made it possible to prevent HIV and manage it with remarkable effectiveness, you’d think health insurance companies would be chomping at the bit to help Americans access these life-saving treatments. But, of course, that would be too easy — and too unprofitable.
Take PrEP (pre-exposure prophylaxis), for example — a medication that can reduce the risk of contracting HIV by up to 99% if taken correctly. Yet, many insurers have thrown up barrier after barrier: requiring pre-authorization (a.k.a., paperwork nightmares), restricting coverage and slapping on high copays that make it unaffordable for many.
And if that wasn’t enough, the Supreme Court has now agreed to review a challenge to the Affordable Care Act’s (ACA) preventive services mandate — the very requirement that insurers cover life-saving services like PrEP at no cost to patients. If the Court sides with the challengers, it could gut access to not only PrEP but also cancer screenings, preventive medications for heart disease, behavioral health counseling, and more.
Barriers to HIV Treatment
And then there’s the case of HIV-1 treatment and management drugs like Biktarvy, which are essential for those living with the virus to maintain their health and reduce the risk of transmission. Rather than ensuring easy access, insurers often categorize these meds as “specialty drugs,” which is code for “ridiculously expensive.”
Patients with private insurance are often left with sky-high out-of-pocket costs or forced to jump through hoops just to get the medication they need to stay healthy. Meanwhile, many insurance companies continue to pad their bottom lines, all while claiming they’re doing everything they can to keep costs down.
To make matters worse, the SCOTUS case could further embolden insurers to make accessing these medications even harder. The legal challenge hinges on whether the ACA’s preventive services mandate, based on recommendations from the U.S. Preventive Services Task Force, is valid. Plaintiffs — including two Christian-owned companies — argue that covering PrEP violates their religious beliefs. The 5th U.S. Circuit Court of Appeals partially sided with them, and now the Supreme Court will weigh in. Should the Court rule against the ACA mandate, insurers could gain even more leeway to exclude crucial preventive medications under the guise of religious or other objections.
Adding Insult to Injury
This all comes after decades of fear, stigma and misinformation surrounding HIV. For years, people lived in terror of the virus, and those living with HIV were shunned and isolated by society. Now that science has finally given patients the tools to prevent and manage HIV effectively, it’s downright reprehensible that some insurers, policymakers and judges are still putting up roadblocks.
HIV prevention and treatment aren’t exactly cash cows for insurers. They’d much rather focus on high-profit, low-risk enrollees and leave those needing costly, life-saving meds to fend for themselves. After all, if they can keep those pesky sick people from draining their resources, their financial standings on Wall Street look all the rosier.
The glimmer of hope is that some policymakers are paying attention. In 2023, Sen. Tina Smith (D-MN) and former Rep. and now Sen. Adam Schiff [D-CA] introduced the PrEP Access and Coverage Act of 2023, which aims to mandate that insurers cover PrEP and related services without cost-sharing or preauthorization. The legislation is a step in the right direction, but its fate is uncertain, especially with the Supreme Court now poised to weigh in on the ACA mandate and a Trump presidency, that could try to repeal numerous ACA provisions.
P.S.
While big health insurers deserve much of the blame some pharmaceutical companies certainly contribute to the high cost of HIV treatment regimens. Drug makers set high prices and maintain them through patents and strategic pricing. The complex interplay between insurers and pharmaceutical companies, coupled with a lack of transparency and competition, keeps HIV drug costs elevated.
All that said, here’s a note for readers who want to get access to PrEP: Don’t be deterred from looking into your options. PrEP is incredibly effective at preventing HIV transmission. Most Americans can now access PrEP for free thanks to a federal mandate under the ACA, still in force, that requires most insurance plans to cover PrEP without any out-of-pocket costs. This includes the medication itself and associated services like doctor visits and lab tests, making it more accessible to those at risk of HIV.
While insurers continue to put up barriers, there are still financial support options available for those in need of HIV treatment regimens. People diagnosed with HIV and in need of expensive medications like Biktarvy or Triumeq can turn to programs from pharmaceutical companies and government initiatives. For instance, Gilead Sciences, the manufacturer of Biktarvy, offers co-pay coupons for those with commercial insurance and Patient Assistance Programs for those without insurance or who are underinsured. Additionally, state-run AIDS Drug Assistance Programs (ADAP) often provide free or low-cost HIV medications for those who qualify.




It's vital that coverage for HIV-related medications be mandatory for all insurers. As soon as SCOTUS reverses that mandate (or, hopefully, does not!), any insurer without such barriers will attract the majority of such patients and have to charge a higher premium, thus becoming less market-competitive. Another race to the bottom that would be prevented with a single national health insurance plan used by all Americans, without this perverse competition.
Disappointing is too mild a word for the state we're in now. After all the strides made in HIV research, now medication to prevent it is at serious risk.