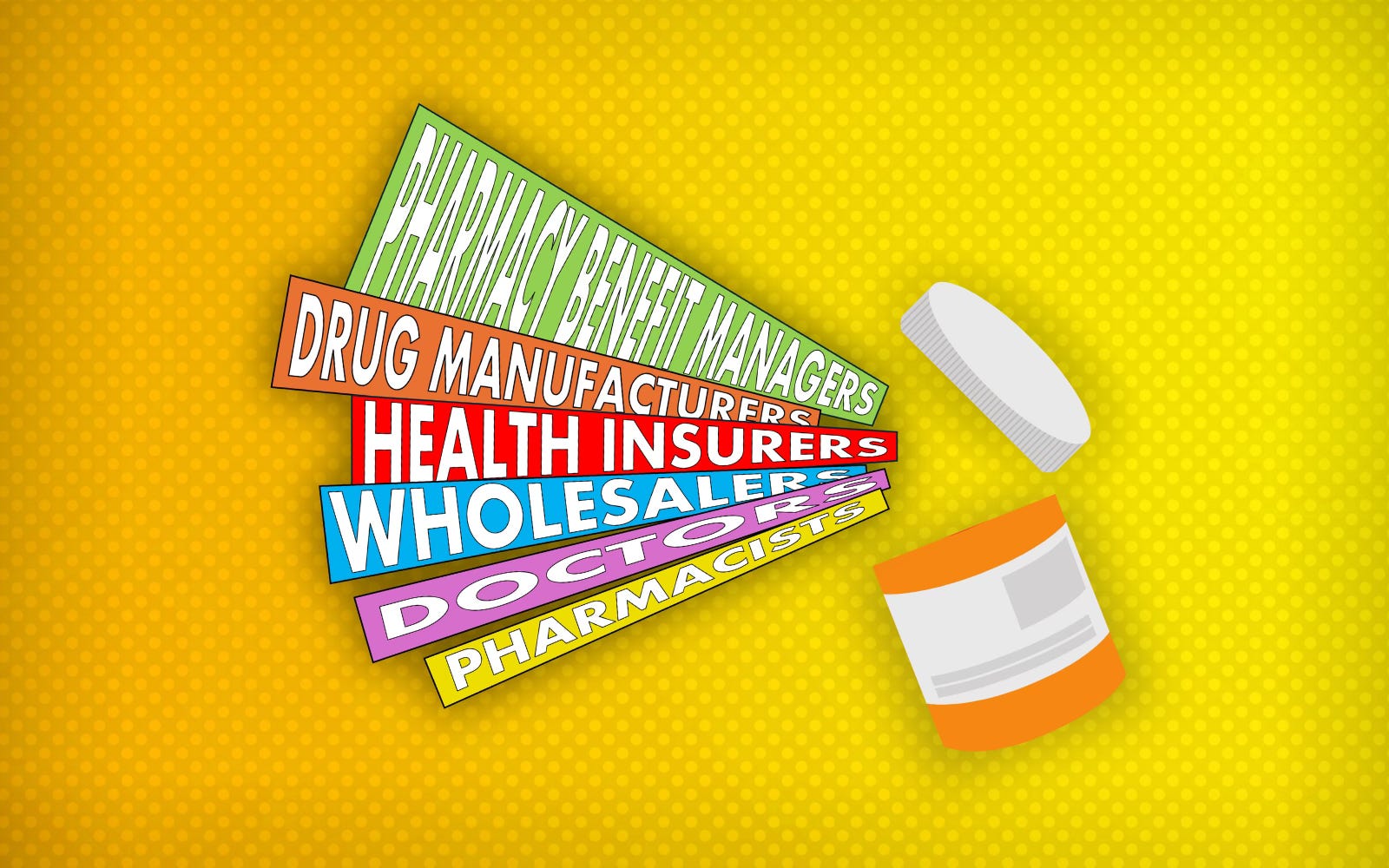
How PBMs Took Over the Prescription Drug Chain — And Left Patients and Pharmacists Paying the Price
PBMs control the cost, the access and the profits. Patients and pharmacists? Just along for the ride.
Editor’s Note:
We’ve published numerous stories about pharmacy benefit managers (PBMs) and how the biggest ones are now owned by a handful of giant health insurance corporations. Many people, though, are just now learning about the central role these middlemen play in determining how much we Americans have to pay out of our own pockets at the pharmacy counter for our meds, even with insurance. So I’ve asked former Columbus Dispatch reporter Lucas Sullivan to write a series of explainers to educate us all, including our lawmakers (maybe especially our lawmakers), on the subject. Lucas has covered this industry for years and has a deep understanding of how PBMs operate and how their business practices affect us as both patients and taxpayers. You’ll want to read every word because there will be a quiz.
-Wendell Potter
Americans spent a record $464 billion last year on prescription drugs, according to recent numbers from the Centers for Medicare & Medicaid Services.
Five years ago that number was $335 billion and a decade ago $298 billion. The dramatic increase is not matched by the number of prescriptions filled by pharmacists during that same span.
The average prescription in 2014 was $69. In 2019 it was $76. In 2024 it was $95. This increase has drawn the ire of Congress, which is calling for reforms. Specifically, officials want to rein in the powers of pharmacy benefit managers (PBMs) and how they set prescription drug prices.
“What PBMs are doing to our health care system is criminal,” said Rep. Buddy Carter (R-Georgia), who was also once a pharmacist.
PBMs are middlemen in the drug supply chain. They are a department within every major health insurer in the United States and profit off nearly every prescription filled. Those on prescription drugs – which is two-thirds of all U.S. adults – don’t ever see or likely talk to their PBM. But since the early 2000s these middlemen have had a crucial role in the price of drugs with little oversight.
A big reason why is the cloaked and complicated medical jargon the industry uses to describe the drug supply chain. Many Americans have their health insurance chosen by their employer. It is up to the employer to decide which plan is best. That decision by CEOs is often dictated by price breaks and incentives offered by health insurers.
So at what point do PBMs become part of the drug supply chain?
(Hint: Doesn’t take too long.)
Drug manufacturers help create, test and get government approval for their drugs. These manufacturers are familiar to many Americans: Pfizer, Johnson & Johnson, Merck, Eli Lilly and Bristol Myers Squibb. In all, there are about a dozen major drug manufacturers.
Next drug manufacturers have to get their drugs on a health insurer’s approved drug list. This approved list is called a formulary. The list contains drugs that offer best health outcomes and the best returns for-profit health insurers, which own the biggest PBMs.
Drug manufacturers offer rebates and discounts to persuade health insurers to list their products on the insurers’ formularies. It’s unclear how much input actual doctors have in the creation of the formulary.
UnitedHealth, the country’s largest and most profitable health insurer, is also the largest employer of doctors in the country. The public knows UnitedHealth’s PBM by the name of OptumRx. This consolidation of the health chain increases the ability of the company to be gatekeepers of prescription drugs, the drug costs and availability for patients.
UnitedHealth has vaulted up the Fortune 100 charts in the last 20 years thanks to this consolidation and now ranks fourth behind WalMart, Amazon and Apple as the country’s most valuable companies. It is valued at $480 billion.
The health insurers and their PBMs also decide if they will allow generics onto their approved lists. To get on these approved lists, PBMs require rebates and discounts from the manufacturers.
Wholesalers purchase the drugs from manufacturers at an already set list price that they have negotiated with the manufacturers.They then distribute the drugs to pharmacies, hospitals and clinics. There are mainly three wholesalers in the U.S.: AmerisourceBergen, Cardinal Health, and McKesson Corporation.
Doctors are largely unaware of the backroom deals health insurers and their PBMs have made with drug manufacturers. Late last year Dr. Bruce A. Scott, president of the American Medical Association (AMA) sounded the alarm that behavior by health insurers and their PBMs are harming patients.
“The call for increased regulatory oversight of PBM business practices is overwhelmingly welcomed by physicians as a check against possible anticompetitive harm resulting from low competition and high vertical integration in the PBM industry,” Scott said.
Pharmacists across the country filled more than 5 billion prescriptions last year. In order to do that they are required by PBMs and health insurers to sign contracts to have access to patients. These contracts give pharmacists little control over the price paid for prescription drugs at their counters. Prices for drugs are set by your health insurer and its PBM. Customers can also pay different amounts for the same drug at the same pharmacy. Why?
Because every health insurer and its PBM works out a different price with the drug manufacturer.
I was allowed behind the counter of an Ohio pharmacy to see what pharmacists see when filling the prescription. On the checkout screen the pharmacist has his or her cost to buy the drug from the manufacturer and what the PBM is expected to be paid by the pharmacist. Per their contracts with PBMs, pharmacists are not allowed to tell patients what those numbers are.
The difference between those two numbers is the spread. The PBM then reimburses the pharmacist a certain amount to provide that drug. Sometimes that reimbursement by the PBM doesn’t cover the pharmacist’s cost to stock the drug.
When government officials began cracking down on PBM spread pricing in 2019 the PBMs pivoted to taking the money back from pharmacists after the transaction occurred. This is known as a clawback.
For example, a pharmacist would put $5 for a blood pressure prescription in their cash drawer and a month later the PBM associated with that patient would send a bill to the pharmacist for $4.59. The pharmacist would get to keep the remaining 41 cents.
How, then, do pharmacists stay in business? They don’t.
An Ohio State University study found nearly 7,000 local pharmacies have closed since 2019 in the United States. CVS pharmacies, however, have not seen such closure rates because they are owned by, you guessed it, the PBM CVS Caremark. And CVS also owns Aetna. From the lab to your pharmacy counter, PBMs have inserted themselves into every phase of a patient’s prescription drug chain. And, based on appearances, the only thing they’ve improved is their profits.
Luke Sullivan has been an investigative reporter for 22 years. Part of The Columbus Dispatch Side Effects investigative team that exposed pharmacy benefit managers. Ohio State graduate. Girl Dad.




Our health care system has been compromised by corporate greed. The mega hospital systems and pharmaceutical companies and the insurance industry. No one has really tried to protect the public. I started working in a university based hospital in the 1970s. The needs of the people most tragically the poor have been ignored. Compared to other countries our healthcare quality statistics are embarrassing. And now the checks and balances we had developed are gone. You know who benefits from this right?
These schemes have been obvious to health care professionals for years, if they bothered to look at the numbers. Formularies have meds with zero copays to patients but what is not apparent is these meds like BP meds, anti cholesterol meds are not free. There are ever increasing charges that insurers and pharmacists are paying for staying in the game. Some meds are almost given away on the formulary as a quid pro quo for carrying certain high priced brand names. Now the generics (which major pharmaceuticals now control) come in two payment tiers! And the formularies are not standard and keep changing coverage as backroom deals are concocted. This makes it very difficult for the average person to make reasonable decisions on which coverage plan to choose.
I personally have an inhaler that costs $300 each and I pay $40 copay. The generic of that inhaler costs me $120 each. I have to insist that my prescriber writes “Brand name only” on my prescription. This makes absolutely no sense. The whole system is corrupted and it is making obscene profits off the illness of the people, who often go bankrupt from medical costs in general. This is not a free market economy, it is a manipulated process by for-profit companies and individuals that are extremely greedy. This is the result of our Congress taking a hands off approach many years ago, for massive payoffs.
And don’t get me started on Advantage Part C supposedly Medicare. The premiums may be free and attractive, but the co-insurance costs are high and the denial rates for treatment are outrageous and deadly.