Big Shifts: CVS Is Pulling the Plug on ACA Coverage — And 1 Million Americans Will Pay the Price
CVS says it can’t make enough money covering a million Americans — just as it celebrates nearly $2 billion in quarterly profits and doubles down on high-dollar weight-loss drugs.
In what’s becoming an all-too-familiar pattern, CVS Health announced it will pull Aetna out of the Affordable Care Act (ACA) marketplace in 2026, leaving about a million people across 17 states searching for new health coverage — and in some cases, fighting to afford any at all.
This marks yet another retreat by a major for-profit insurer from a program designed to provide affordable health coverage to Americans who don’t get it through work. CVS made the announcement while simultaneously celebrating a 60% increase in quarterly profit and revealing a new deal to boost sales of the pricey weight-loss drug Wegovy through its pharmacy and pharmacy benefit manager (PBM) arms.
Let me repeat that: Aetna is exiting the ACA because it claims it can't make enough money on people enrolled in those plans, on the same day its parent company posted nearly $1.8 billion in profits in just the first three months of this year.
This is the same company, by the way, that dumped hundreds of thousands of seniors and disabled people at the end of 2024 because some of them were using more medical care than Wall Street found acceptable. If this doesn’t tell you everything you need to know about who the health insurance industry is really working for, I don’t know what will.
From “Commitment” to Abandonment
Aetna first bailed on the ACA exchanges in 2018, then re-entered in 2022 when insurers could see more clearly how they could make significant profits on that book of business. Now, after just a few years of moderate participation, it’s heading for the exits again. CVS Health executives blamed “regulatory uncertainty” and “highly variable economic factors,” according to a statement to The Columbus Dispatch. But make no mistake—this was a cold business calculation. Uncertainties and economic variabilities are constants in the insurance game.
CVS’ CEO David Joyner told investors:
“We are disappointed by the continued underperformance from our individual exchange products … this is not a decision we made lightly.”
That’s corporate-speak for “our Wall Street friends weren’t impressed.”
Aetna’s ACA exchange business, covering roughly 1 million people, is just a sliver of CVS’ overall medical membership of 27.1 million. But even though the profits weren’t massive, the people depending on this coverage — many of them self-employed, working multiple part-time jobs, or recently uninsured — will now be thrown into chaos.
And it’s happening at a time when health insurance for many Americans hangs by a thread. Unless Congress acts in the coming months, the ACA’s enhanced tax subsidies—first implemented under the American Rescue Plan—are set to expire at the end of this year. Without them, premiums could spike by 50% to 100% depending on income and geography.
The Congressional Budget Office projects that the lapse in subsidies could leave 3.8 million more Americans uninsured — and now, 1 million more will be forced to find new plans as CVS/Aetna walks away.
Same Song: Prioritizing Profit, Not Patients
Let’s be clear about what CVS is doing here: It’s ditching an essential safety net for millions in order to chase higher profits elsewhere—most notably, in the exploding market for GLP-1 drugs like Wegovy. On the same day it abandoned the ACA, CVS announced a new deal to give Wegovy preferred placement on its PBM formulary, displacing Eli Lilly’s Zepbound. This will help CVS dominate the obesity drug market—and rake in profits through its Caremark PBM and nearly 9,000 retail pharmacies.
It’s a powerful example of vertical integration in action. CVS owns the insurer (Aetna), the PBM (Caremark), and the pharmacy (CVS retail stores). When it walks away from lower-margin business like ACA plans and doubles down on high-dollar drug deals, we see its true priorities: selling expensive drugs, saddling individuals, families and employers with the costs, and keeping Wall Street happy.
Even worse, the decision is taking place against a troubling political backdrop. The Trump administration has already taken steps to undermine ACA infrastructure and expressed skepticism toward core public health programs. Cuts to navigator funding, changes to vaccine guidelines, and looming uncertainty around tax credits are all part of a slow-motion sabotage of the ACA. This is not to say that the ACA doesn’t have its flaws that need to be addressed. But instead of penalizing hard-working Americans and their families, lawmakers and the Trump administration should focus instead on lowering the ridiculously high out-of-pocket maximum that the ACA established (and that keeps going up every year) and fixing the medical loss ratio provision that has fueled the vertical integration in the insurance industry.
CVS executives didn’t mention politics in their earnings call. But make no mistake: this exit is happening in a climate in which subsidies that enable people to afford their premiums are in doubt. CVS is cutting and running, just as millions of Americans may need the exchanges more than ever.
CVS Isn’t Just Shifting in the ACA — It’s Happening in Employer Plans Too
CVS’s quiet reshuffling of coverage priorities seems to not just be limited to the ACA marketplace. The company is also steering employer-based plan members — people who get their insurance through work — toward CVS-owned services.
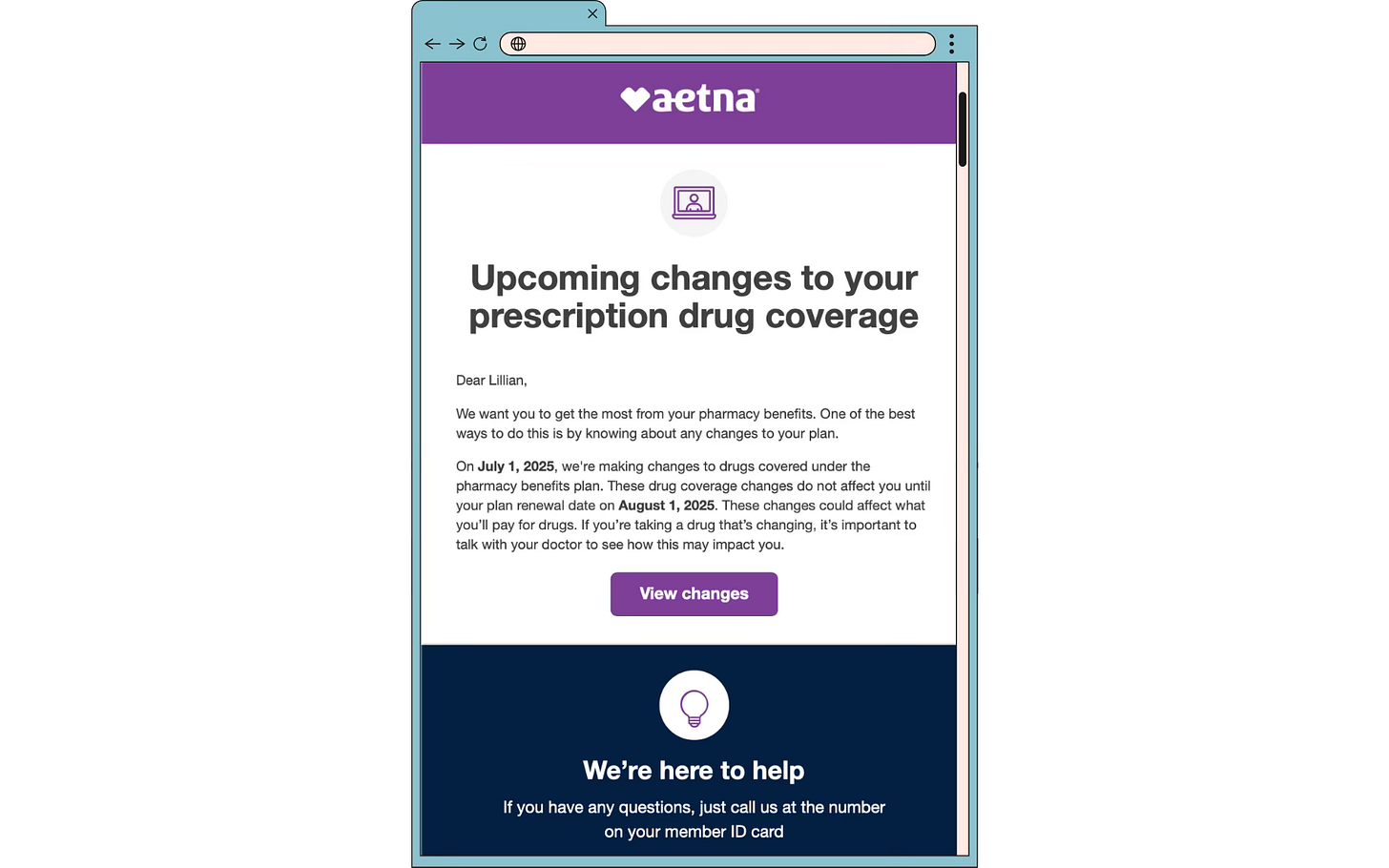
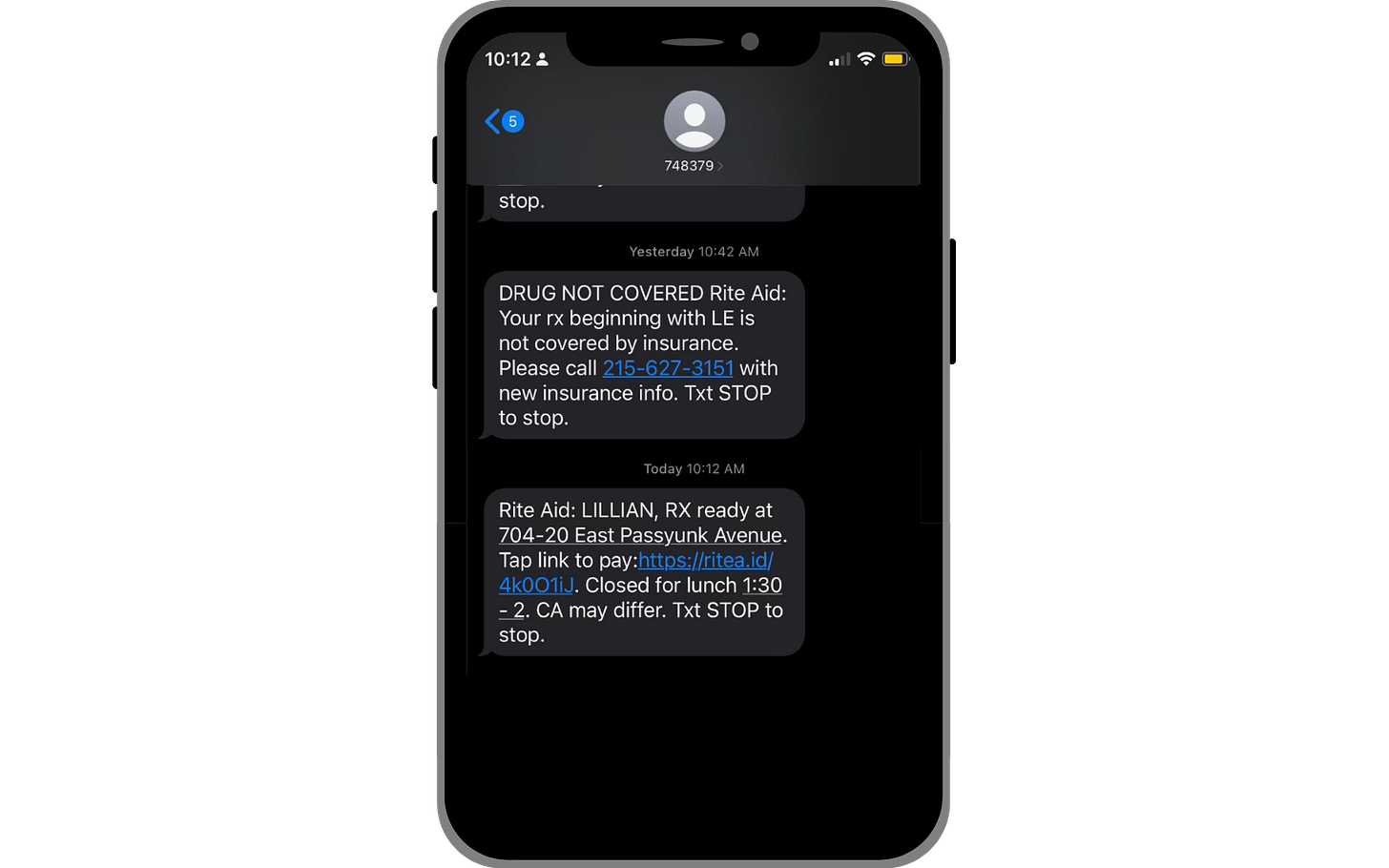
Take, for example, Lillian Hurley, a 31-year-old Philadelphia woman enrolled in an Aetna plan through her employer. She recently received a notice from Aetna informing her that, starting this summer, her medications would no longer be covered at her current pharmacy. To continue receiving coverage for her medications, she would need to switch to a CVS pharmacy – one affiliated with Aetna.
This is more than a logistical hassle. It’s a reflection of how vertically integrated health care giants like CVS/Aetna use their scale not just to dictate what care gets covered, but where and through whom you’re allowed to get it.
For Hurley — and many others — it’s a reminder that corporate consolidation isn’t just about stock prices and strategy decks. It affects people’s lives in deeply personal ways.
When insurers, PBMs, and pharmacies are all owned by the same corporation, patients lose. They lose choice, they lose control, and all too often, people lose access.
This is why transparency, accountability, and public oversight aren’t just buzzwords. CVS says it wants to be "the most trusted health care company in America." But trust is earned, not declared. You don’t earn it by pulling out of programs that help the most vulnerable. You don’t earn it by prioritizing billion-dollar deals over basic access to care.






MKBroker you speak like a broker. Cold and calculating. The medical economy is not just about profit and loss.
Your “flawed premise” is that health care should generate profit the way other corporate sectors generate profit. The flawed premise is that free market capitalism can fix the problem of health care access in this country.
If 1.8 billion quarterly is not satisfactory profit for private enterprise, then we need to nationalize.
When things fall apart after they gut Medicaid we will have to pick up the pieces as a Nation.
Mark my words: all the INSCOs will get out of health care when it is no longer profitable to the degree the shareholders deem adequate.
We the people will be left holding the bag.
This news is abominable. Once again we need Medicare for All, and dump all of these private insurance companies. Health care is a obligation of the United States Government to take care of its citizenry, and the first rule is that the Government sets the costs, and these profiteering companies have to deal with it or get out like Aetna is doing, leaving a million or more people scrambling to get health care in this allegedly richest country in the world that let's its People go bankrupt because skyrocketing costs (short-term profits) are the only goal of these companies; it is certainly not the health and care of patients. It is high time the US Congress and especially the Senate pull the plug on Medicare Advantage privatized policies and start to live up to the goals that are the contract with the American People. We are an embarrassment to the rest of the World as far as a so-called Super Power that cannot even manage to bring down medical and pharmacy costs will sucking on the teats of the Health Insurance and Big Pharmaceutical lobbies. We have become a 4th World country and that is unconscionable. It's clear that this Administration by its selection of a lousy Health Secretary who has profited from his anti-vaccine stance that health care in practice is not considered part of the overall National Security of this country, but subsidizing our bloated defense budget is the only hold on power that we have left, since Trump seeks to over turn democracy. What a shame of a Nation we have become.